This blog was written by Jenn Sharman RMT.
Jenn is the owner of Intent Health Clinic in Vancouver, BC. She is a passionate advocate of evidence based practices.
I am sharing it to you with her permission.
“I was in a car accident last year and my Doctor recommended Registered Massage Therapy. I felt anxious about going for a massage but I wanted to give it a try. I knew it was going to be hard for me to talk about the areas of my body that I didn’t want touched or massaged. My Doctor suggested I look for a ‘Trauma Informed RMT’. I didn’t even know that was a thing!
Finding a Trauma Informed RMT made a world of difference. My RMT didn’t ask for details about why it was hard for me to get a massage – they just accepted me as I was and worked with me to find ways I could feel comfortable. My RMT was a great listener. They asked me about my boundaries and preferences and told me it was okay if those changed from day to day. They helped me make choices about how our treatment would go each time, so there were no surprises. I knew I could trust them and it helped me feel more relaxed. I came to really enjoy my massage appointments!”
What Is Trauma?
According to the Trauma Informed Practice Toolkit: “individual trauma results from an event, series of events, or set or circumstances that is experienced by an individual as physically or emotionally harmful or life threatening and that has lasting adverse effects on the individual’s functioning and mental, physical, social, emotional or spiritual well-being.”
Trauma may result from adverse childhood events such as abuse, neglect and disrupted attachment, and at any stage of life through acts of violence, accidents, medical procedures, natural disasters, war, sudden unexpected loss and systemic oppression. Trauma can be due to direct individual experience or it may be historical and intergenerational in nature.
“How people are affected by trauma they experience depends on many different factors including what their life and relationships were like before the trauma happened, how people responded to them during and after the trauma, their own personality, strengths and resources, their other life experiences and the cultural context in which they live their lives” (TIP Toolkit).
How Common is Trauma?
The experience of traumatic events in childhood and adulthood is all too common. 76% of Canadian adults report experiencing a form of trauma and an estimated 9.2% meet the criteria for diagnosis of Post Traumatic Stress Disorder (PTSD) (Ameringen, 2008).
Experiencing trauma can directly impact a person’s health and their comfort in interacting with healthcare providers. People who have experienced trauma may develop chronic pain, headaches, stress, insomnia, anxiety, depression or PTSD. Research demonstrates a correlation between childhood abuse and chronic pain syndromes (The Sensitive Practice Guide).
Trauma can impact a person’s memory and brain development, their sense of safety, their ability to ask for help and voice their preferences, their capacity to regulate emotions and to experience trust in relationships. Considering the prevalence of trauma and the wide-reaching impacts, we can understand how important it is for RMTs to apply the principles of trauma-informed practice in their role as health care providers.
A trauma-informed approach fosters trust, safety, clear communication and collaboration and reduces the chances of inadvertently causing additional harm.
Information and care provided in a trauma-informed manner is beneficial for all patients/clients and should be applied as a universal standard of care, regardless of trauma history or disclosure.
“Utilizing a trauma-informed approach does not necessarily require disclosure of trauma. Rather, services are provided in ways that recognize the need for physical and emotional safety, as well as choice and control in decisions affecting one’s treatment. Trauma-informed practice is more about the overall essence of the approach, or way of being in the relationship, than a specific treatment strategy or method.” -TIP Guide
What Is Trauma Informed Massage Therapy?
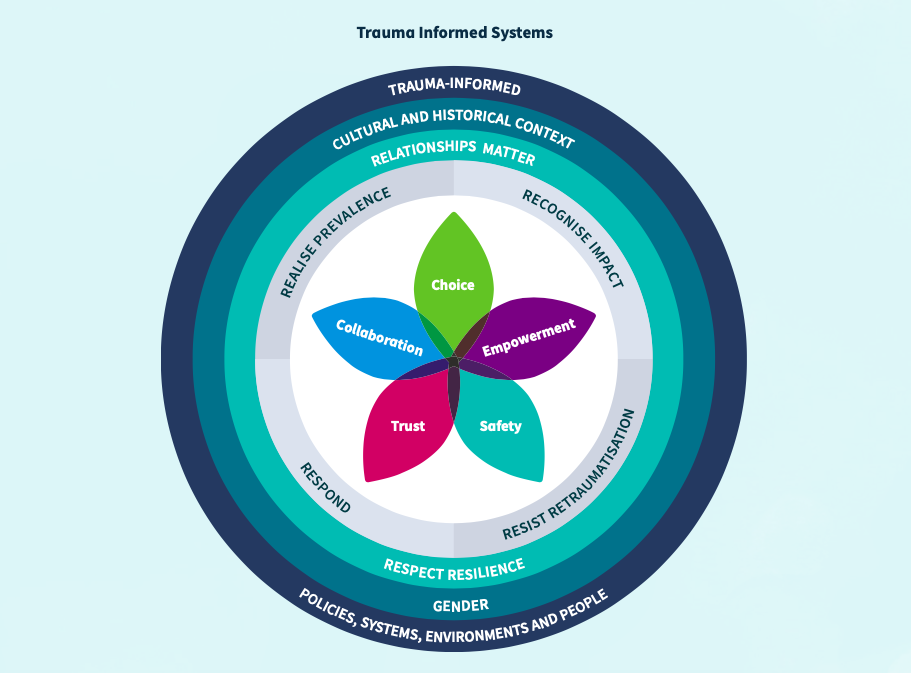
When an RMT has a Trauma-Informed Practice, they follow these four principles:
- Trauma Awareness
- Safety and Trustworthiness
- Choice, Collaboration and Connections
- Strengths-based skill building
1. Trauma Awareness: the RMT is aware of the impacts of trauma and the adaptations people may make to cope and survive after trauma. They use language that de-stigmatizes and normalizes an individual’s responses to trauma. Reactions such as lack of motivation, anger, irritability, avoidance of appointments or resistance to treatment can be reframed as survival mechanisms that are triggered by a perceived threat(s). This understanding can help to depersonalize challenging interactions and increase a practitioner’s ability to stay present and empathize while demonstrating healthy professional boundaries. Awareness of trauma does not mean that the RMT has to be an expert on trauma, it means that they are able to recognize possible trauma responses and respond appropriately.
“My RMT noticed when I started to feel uncomfortable and checked in with me right away. I felt embarrassed for having a reaction and I wasn’t sure if they would want to see me again. My RMT told me that it was normal to feel anxious and reassured me that they still wanted to work with me if I wanted to continue. That really felt good because I knew they accepted me despite my difficulties.”
2. Safety and Trustworthiness can be established through practices such as a welcoming intake process, adapting the physical space to be calm and non-threatening (consider noise levels, style of decor, layout of space), demonstrating an interest in the patient’s experience and narrative, providing clear information, engaging in active listening, ensuring informed and enthusiastic consent and creating a reassuring predictability in both the treatment space and the treatment itself. Communicating professional boundaries with a positive regard for the patient can create a framework of clarity and respect (ending the treatment on time, secure draping, etc.) that contributes to feelings of safety.
“I often feel stressed out when I’m in the waiting area at my Doctor’s office, not really knowing what will happen or how long it will take. At my RMT’s clinic I feel more relaxed when I walk in. The atmosphere is calming with soft music, plants and nature photographs. I know they will ask me questions about how I’m feeling and how I want the massage to go that day. I just like knowing what to expect. I can relax more.”
3. Choice, Collaboration and Connections are established through interactions that foster self-efficacy, self-determination and empowerment for those receiving care. This could involve asking about treatment preferences; what has worked for the patient in the past; identifying areas of their body that are off limits for treatment that day; or if there are areas where contact can now be explored, and how. It can involve checking-in during the massage to see if needs and expectations are being met. At the same time, it is important to be mindful of not checking in too often, and perceiving when too many options/choices could be overwhelming to the patient.
“At first it was really hard for me to even know what my body was asking for. My RMT was patient in talking about the different choices I could make about the treatment that day. We would always chat after the massage about what worked for me, and if there was anything I would try differently next time. Sometimes I didn’t know. We didn’t always get it right, but what mattered was that they cared about my experience and were open to making changes as we went along.”
“By demonstrating respect for and sensitivity to personal boundaries, clinicians model healthy boundaries and reinforce patient’s worth and right to personal autonomy.” -The Sensitive Practice Guide
4. Strengths-based skill building involves assisting patients to identify their strengths to further empower self-efficacy and resiliency. It involves skillfully reframing from a strengths-based perspective. For example, an RMT can ask questions about self care practices that are working for the patient, and what their strengths, interests, goals, and skills are in order to empower and build capacity for self-care.
“There were some days where I was feeling pretty depressed and thinking I might not get better. My RMT helped show me the progress I had made in strengthening my body. They weren’t overly cheerful about it. They knew it was hard for me on those days, but they had a gentle way of chatting about the successes I had in the past. We set goals together that were realistic and meaningful for me.”
Personal Growth As A Trauma Informed RMT
RMTs working in a trauma-informed manner recognize the importance of self-reflection and processing their own personal trauma history as well as practicing self-regulation strategies. Seeking support through counselling or reflecting with a mentor can be extremely valuable as RMTs learn and continue to apply a trauma-informed lens. Further learning about co-regulation of our nervous systems, attachment theory, transference, countertransference, anti-racism and unconscious bias is extremely valuable. The Trauma Informed Practice Guide contains questions for self-reflection as well as grounding exercises.
Remember, you don’t need to be an expert on trauma to apply the principles of trauma-informed practice. Learning about trauma-informed approaches is a life-long journey that provides a structure for safety and growth on many levels: personally, professionally, within our families and within our communities.
Every interaction a Registered Massage Therapist has with a patient is an opportunity to cultivate trust, safety, clear communication, collaboration and choice.
References And Further Learning:
Trauma-Informed Practice Guide. Published May 2013. Accessed June 2021.
Trauma-Informed Practice Toolkit. Scottish Government. Published: March 2021. Accessed June 2021.
Van Ameringen, M. et al. Posttraumatic stress disorder in Canada. CNS Neuroscience & Therapeutics, 2008. 14(3): 171-181.
The Sensitive Practice Guide. Published 2009. Accessed June 2021.
Interested to continue your professional development with ongoing monthly webinars and research reviews?
When you join the Manual and Movement Therapists Community (MMTC) you will receive exclusive access to professional development you want and regular research reviews and discussions to help you become the best therapist possible.
This is all delivered within a positive, supportive and members only environment!
Click on the image below to learn more!