I am really proud to share this article with the massage therapy and MSK professions. Below is a copy of the published text. If you want a free PDF copy which includes a full reference list, please click on the link below ↓
Download a free PDF of the full article here
This link below will give you a PDF booklet of the 5 Key Takeaways from our article.
Massage Therapy A Person-Centred Approach to Chronic Pain (1)
Massage Therapy: A Person Centred Approach to Chronic Pain
Authors: Richard Lebert, RMT, Monica Noy, MSc, RMT, Eric Purves, MSc, RMT, Jacqueline Tibbett, PhD, LMT
Person-centred care is an emergent movement within evidence-based medi-cine that has the potential to transform the health care system. Person-centred care is a collaborative approach in which health care professionals partner with patients to co-design and deliver personalized care with a focus on physical comfort, emo-tional well-being, and patient empower-ment. By embracing person-centred care through two-way communication, patient engagement, and self-management strat-egies, massage therapists have the poten-tial to further reduce suffering associated with chronic pain in our society.
INTRODUCTION
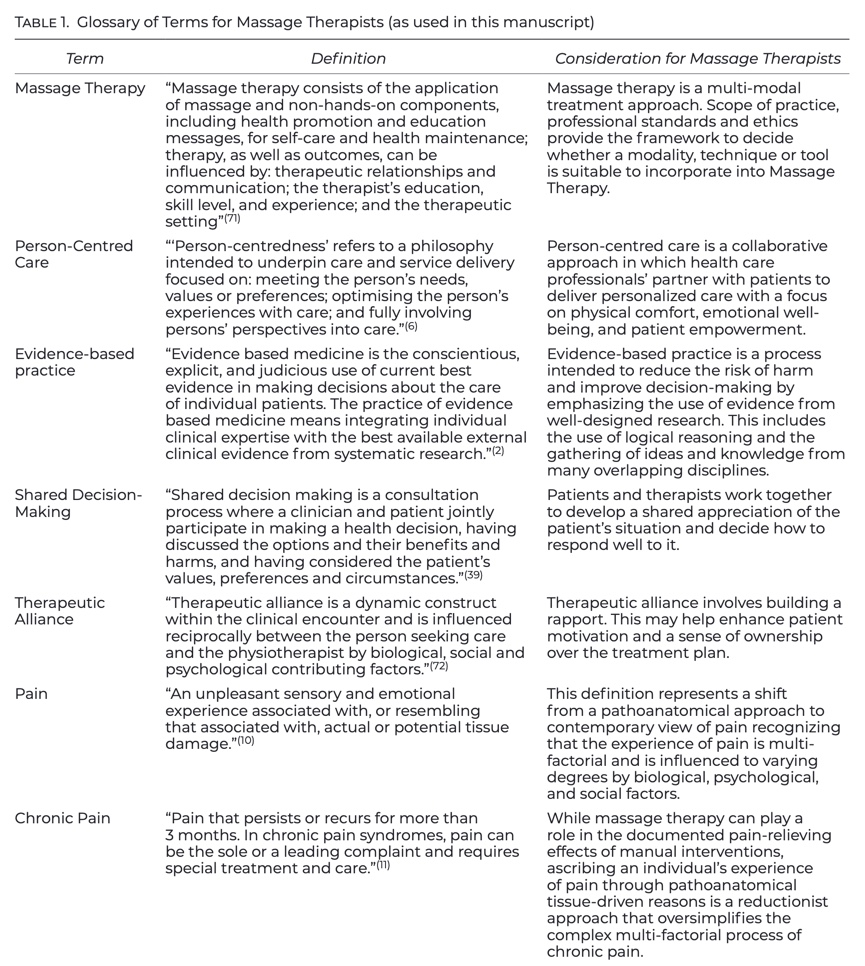
A Person-Centred Approach as an Enhancement to Evidence-Based Medicine
In the 1990’s, David Sackett and Gordon Guyatt introduced evidence-based medicine as the conscientious use of current best evidence in making decisions about patient care. Evidence-based medicine (also known as evidence-based practice) is a process intended to reduce the risk of harm and improve decision-making by emphasizing the use of evidence from well-designed research. This includes the use of logical reasoning, and the gathering of ideas and knowledge from many overlapping disciplines. The enduring contributions of this movement are three principles of evidence-based practice (best available evidence, clinical expertise, and patient values) that are transforming health care. A definition of terms is provided in the Glossary of Terms for Massage Therapists (Table 1).
Evidence-based practice is a cohesive approach with a goal of improving patient outcomes. It is a key indicator of high- quality patient care, but some have argued that individual patient values and goals are often undervalued. In response, another emergent movement that has the potential to transform the health care system is the implementation of person-centred care.
Person-centred care is a collaborative approach in which health care professionals partner with patients to deliver personalized care with a focus on physical comfort, emotional well-being, and patient empowerment. Person-centred care is an approach that serves to reorient perspective towards the individual, and it places an emphasis on shared decision-making based on the individual’s circumstances. In this article we explore person-centred clinical reasoning, according to the ideals of evidence-based health care, for the profession of massage therapy.
Treatment for Chronic Pain
The International Association for the Study of Pain (IASP) states that “pain is an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.” The definition of pain was changed in 2020 to indicate that pain is an experience that is unique to the person and that should be respected even if the source of pain is not identified. This change corresponds with an evidence-based shift away from a pathoanatomical (‘structural’) focus on pain treatment that includes recognizing the experience of pain is multi-factorial and is influenced to varying degrees by biological, psychological, and social factors.
Chronic pain is defined as pain that persists or recurs for more than three months and is highly prevalent (affecting an estimated 30% of people worldwide). Individuals suffering from chronic pain can be poorly served with conventional pain management interventions. Medical treatment options for chronic pain include opioids, corticosteroid injections, and arthroscopic and other invasive surgeries. These interventions carry a considerable risk for adverse events and, when compared to placebo, have minimal efficacy for people experiencing chronic pain. The current medical landscape and the high impact of chronic pain present a need to develop effective evidence-based strategies. Doing so may require reevaluating long-held assumptions that relate to the assessment and treatment of people experiencing chronic pain.
Caring for individuals by way of chronic pain management is shifting away f rom a pathoanatomical approach to one that prioritizes function and quality of life, rather than complete pain relief. As part of this shift, clinical decision-making ought to reflect the understanding that structural abnormalities alone do not explain or necessarily predict pain. A person-centred approach acknowledges that patient presentation and recovery is variable and is based on the understanding that biological, psychological, and social factors are integral to the experience. Instead of focusing primarily on pathoanatomical structures, both clinicians and patients work together to improve function and quality of life.
Evidence Supports a Person-Centred Approach to Chronic Pain
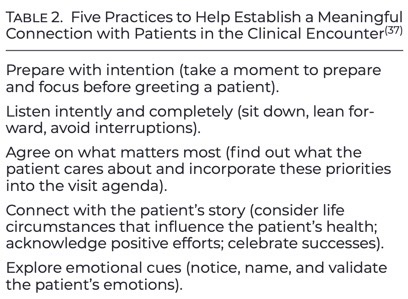
A person-centred approach is one that seeks to understand better the dynamic between biological, psychological, and social factors. This information is used to formulate a clinical hypothesis that does not seek a sole source of pain. If adopted widely, a person-centred approach to care helps massage therapists understand the complexity of the person’s pain experience, leading to improved patient–therapist relationships, improved self-efficacy, and better health outcomes for people with chronic pain. A clinical assessment is a key step in this process as it helps establish a meaningful connection and aids clinical decision-making based on patients’ limitations, goals, course of pain, and prognostic factors for delayed recovery. Listening to the personal narrative can help the massage therapist and patient identify meaningful goals, and shared decision-making can help to identify the most appropriate intervention based on pain presentation, functional limitations, and psychosocial factors. A quick guide to practices that help establish connection within the clinical encounter is provided in Table 2. The distinguishing marker of person-centred care is that it nurtures a supportive relationship, emphasizes two-way communication, and empowers patient participation in health care decisions. The added value of a person-centred approach is that, even when underlying mechanisms are unclear, by understanding an individual’s functional limitations and how pain is affecting their activities of daily life, the practitioner can still formulate a meaningful treatment plan. This is accomplished by using shared decision-making in which patients and massage therapists work together to develop a shared appreciation of the patient’s situation and decide how to respond. Shared decision-making involves three key actions: recognizing and acknowledging that a decision is required; knowing and understanding the best available evidence; and incorporating the patient’s values and preferences into the decision.
DISCUSSION
Applying a Person-Centred Approach to Massage Practice
Massage therapists see themselves as empathetic health professionals who focus on therapeutic relationships, individualized care, and patient empowerment. It is because of these values in the profession that massage therapists are well-suited to deliver person-centred care for individuals experiencing chronic pain. There are many ways that massage therapists could apply person-centred care. Here we will expand on three strategies that massage therapists can achieve this: 1) using person-centred communication and shared decision-making; 2) facilitating health literacy and patient engagement; and 3) promoting the use of active self-management strategies.
1. Using person-centred communication and shared decision-making
Communication is as important as any manual intervention massage therapists perform. The combination of manual therapy with a dethreatening explanation provided in a safe and supportive context can be a powerful analgesic. Effective communication is also fundamental for shared decision-making; clinical practice guidelines for chronic pain emphasize the importance of shared decision-making and a discussion of risks and treatment options. To provide easy-to-understand and accessible information, massage therapists should avoid the use of medical jargon and embrace the use of patient education and decision aids to facilitate an evidence-based understanding of treatment options and enhance patient understanding. Incorporating positive narratives that reassure and educate the patient are consistent with current best practices. When used correctly, language is a tool to enable and encourage; when used incorrectly, language may contribute to the maintenance of their pain state. The massage therapist must be careful to avoid language that is overly pathoanatomical and suggests damage and poor prognosis, such as musculoskeletal components being “out of alignment” or “weak”. This type of language can elicit nocebo effects, creating feelings of brokenness, damage, weakness, and fragility. The long-term effects that health care providers’ language and beliefs can have on their patients must be considered with every patient interaction; this impact is well-established in the literature.
2. Facilitating health literacy and patient engagement
It is important that massage therapists have access to educational resources that are evidence-based. Choosing Wisely (ChoosingWisely.org) and Wiser Health-care (WiserHealthcare.org) are organizations that provide resources for massage therapists and patients about low value interventions which are no longer recommended for people with musculoskeletal pain based on current research. These are resources that can aid patients and massage therapists as they engage in shared decision-making when choosing treatment options for musculoskeletal pain. A positive therapeutic alliance based on empathy and mutual trust can improve treatment adherence and amplify benefits from the actual treatment. Developing therapeutic alliance helps with adherence to the treatment plan and may keep patients engaged with self-management strategies. Reframing care from the pathoanatomical to a person-centred supportive self-management approach has the benefits of a positive therapeutic alliance and patient empowerment.Therapeutic alliance can be used to shift patient expectations and set realistic, individualized goals that prioritize function and quality of life.
3. Promoting the use of active self-management strategies
Physical activity and exercise programs may play a role in decreasing the socio-economic burden associated with chronic pain. Physical activity has been shown to reduce symptoms of anxiety and pain, and to improve function. Additionally, most forms of low-impact physical activity, such as walking, Pilates, Tai Chi, yoga, or aquatic therapy, are considered safe and beneficial for health in people with multiple comorbidities. The World Health Organization recommends healthy adults should undertake 150–300 min of moderate-intensity, or 75–150 min of vigorous-intensity physical activity, or some equivalent combination of moderate-intensity and vigorous-intensity aerobic physical activity, per week. These guidelines highlight the importance of physical activity (both aerobic and strengthening activities), and emphasize the value of any activity, of any duration, and any intensity. Exercise programs for people with chronic pain should take into account peoples’ specific needs, abilities, and preferences. There may be hesitancy to setting up a program; however, here are some suggestions that may be useful for people with chronic pain. Start low and go slow (e.g., 5 min every other day) and aim for a moderate level of intensity. Use a graded activity approach—add 10 min every three to four weeks, towards a goal of 30 min of exercise five days a week. If you don’t know where to start, pick low impact physical activity, such as walking, Tai Chi, yoga or aquatic therapy. In the end, the key to effectiveness of exercise is adherence, so keep in mind people with chronic pain should be encouraged to perform the exercise that they enjoy to promote adherence. Massage therapy could play a supportive role in promoting physical activities, particularly ones that the individual finds enjoyable and meaningful. Scope of practice, professional standards, and ethics provide the framework to decide whether a modality, technique or tool is suitable to incorporate into a massage therapy treatment plan. When local licensing and scope of practice allows it, exercise may be included as part of a treatment plan to help patients actively manage their pain.
CONCLUSION
Improving the way chronic pain is treated and managed by massage therapists is essential for improving treatment outcomes. Contemporary best-practices for pain care support a multi-dimensional approach that understands the intersection of biological, psychological, and social factors and empowers people with shared decision-making. Providing a person-centred approach that includes evidence-based practice and shared decision-making facilitates self-efficacy and is of paramount importance for massage therapists. Embracing a person-centred approach can help to reorient perspective towards the individual and tailor treatment plans based on each patient’s unique values.
Key Takeaways


1. Choose words carefully: avoid overly pathoanatomical language that implies a person is damaged.
2. Facilitate a trusting relationship through connecting with a person’s story and emotional cues, and their val- ues and goals.
3. Consider the use of patient education and decision aids that encourage health literacy.
4. Use high quality, evidence-based re-sources and shared decision-making with the patient.
5. Promote the use of self-management strategies, such as participation in physical activity, that are enjoyable and meaningful to the individual
ACKNOWLEDGEMENTS
RL created the concept and wrote the first draft. JT, MN and EP revised, improved, and rewrote the first draft. All authors contributed to the article and approved the final version of the article.
CONFLICT OF INTEREST NOTIFICATION
The authors declare there are no con- flicts of interest.
COPYRIGHT
Published under the CreativeCommons Attribution-NonCommercial-NoDerivs 3.0 License.
REFERENCES
A full list of references can be found in the official article.