The chances are you will have experienced an episode of low back pain at least once in your life. You’ve probably experienced it many times. Low back pain is one of the most normal things a human can experience. It’s estimated in some studies that over 80% of people will get an episode of back pain at least once every 2 years. The global burden for spinal pain results in more disability, functional losses and loss of work than conditions like diabetes or cancer. The actual burden of spinal pain is increasing every decade! This can be seen in this very busy looking but informative chart.
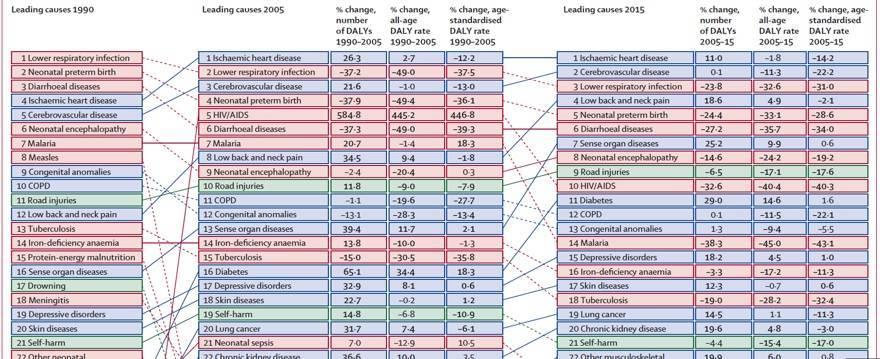
I often present this chart in the courses I teach and I ask participants this question, “why do you think low back and neck pain has moved up from the 12th largest burden of disease to the 4th in 25 years?” To clarify, I don’t like thinking of spinal pain as a disease. By definition, spinal pain could be a disease, “a disorder of structure or function in a human, animal, or plant, especially one that produces specific signs or symptoms or that affects a specific location and is not simply a direct result of physical injury.” However, when people think of a disease, they envision an invading pathogen, tumour, heart disease or an autoimmune condition. By labelling back pain, a very normal occurrence in all humans, as a disease it may lead to further pathological thinking. How we think shapes our communication and influences how we act. Words matter, and they matter a lot! Therefore, when we are discussing spinal pain we should be mindful of how we communicate and the influence this could have on patient and societal attitudes.
Some of the most common responses I get from my question above are; humans are more sedentary, they sit at computers, are overweight, or experiencing higher stress levels now. These things will play a role, but I don’t think they are the most important factors to consider. I think a bigger problem with spinal and neck pain is that as a society we have made it something that people should fear. People think they shouldn’t have pain, or if they do there must be something structurally wrong that needs to be fixed. To make this matter worse, let’s pause for a moment and think about what new technology or interventions are more widely used now than 25-30 years ago?
Searching for a problem
Early spinal imaging is not recommended for spinal pain by both US and European clinical practice guidelines (Wong & Johnson, 2012). MRI’s are associated with more back pain interventions and no better outcomes for non-specific low back pain (Hayden et al, 2005). Availability of spinal surgeons is associated with more back surgeries, I know I need a reference here, but I cannot seem to find where I got this statement from?
When there is a search for something wrong, there is increased likelihood you can find a perceived pathology, structural or movement abnormality. Humans aren’t symmetrical, our discs bulge, our joints change, we do not always move in predictable patterns. That is okay, that is normal. The use of medical imaging or structural based physical examinations to diagnose or make a clinical decision to suggest a fix is unnecessary. This line of reasoning reinforces the belief that pain must have a structural cause which can further aggravate the suffering for many low back pain sufferers. There are suggestions that the more we treat low back pain, the worse the outcomes are (Deyo et al, 2009).
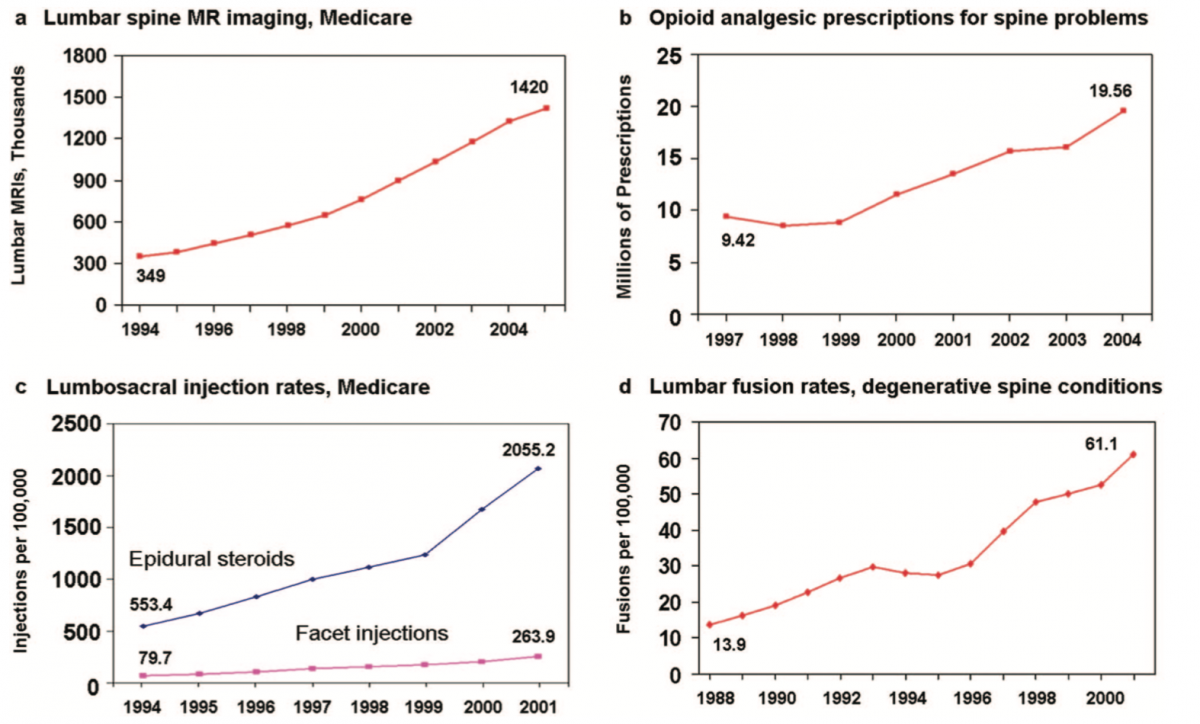
This is a great graph highlighting the increases in spinal imaging, opioid presciptions, injections and spinal fusion surgeries from the late 1980’s to early 2000’s. This data correlates strongly with the graph above. We need to be careful inferring causation among data sets, but it is plausible that a strong relationship exists.
Pain vs Suffering
Before we move on, a distinction between pain and suffering needs to be made. This can become a bit esoteric of a conversation but I think it is important in this context. To suffer is to experience something bad or unpleasant. It adversely affects your well-being. I think of this as the difference between disease and illness. The disease is the physical thing that is wrong with you, ie an infection, diabetes, a cardiovascular problem. Illness is the behaviours that often occur because of the disease. As manual therapists, the illness behaviours is what we need to address so our patient’s can manage.
What did our grandparents do?
Is there something about our modern way of life which makes back pain worse? Has pain become more widespread over the past couple centuries? I don’t think so. I don’t think the data backs that up either. The difference we see today is more suffering and pain related disability. More people may suffer from back pain today, but the actual experience of back pain is nothing new. Back pain is a universal experience that is as old as humankind. All cultures experience it. One thing I always like to ask participants in my courses, and I also ask this of certain patients, ‘what would grandma and grandpa do?’ Was back pain something that routinely debilitated them or others of their generation?
Yes, back pain has a long history of negatively impacting well-being. Seeking compensation for back pain is nothing new either as ‘railway spine’ was a common thing in the 1800’s. The mechanism of pain and perceived injury is similar between railway and automobile accidents. The current understanding is that the prolonged pain related disability and suffering is more related to PTSD and other BPS variables rather than tissue injuries.
In our grandparents generation, if they had back pain, most would get on with life as best they could until it diminished. It ran its course and life returned to normal with no long-term consequences. Why? My assumption is because being disabled and suffering wasn’t an option for them. One thing I learned from my grandparents was, “if you don’t show up to work, you don’t get paid, regardless of how terrible you feel!” There wasn’t much anyone could do for low back pain anyway as the treatment options were limited to either rest, aspirin or laudanum.
Our grandparents, and great grandparents had a great term for low back pain, lumbago. Regular ol’ back pain had a fancy name. I wish it was still in use. However, I can imagine if it was used today it would be promulgated as some pathological disease of the lumbar spine. ‘Oh no dear, I have contracted the lumbago, the doctor says I only have weeks to live!’
I am not trying to diminish the severity of low back pain sufferers. Of course back pain is very real and very crippling for so many people. Trying to make light of it is not meant to undermine the suffering that people experience. Persistent spinal pain negatively impacts so many, but it doesn’t need to. If we followed the research of the past 40+ years we would better appreciate various pain mechanisms and better care could be provided to those who hurt. I am someone that routinely gets bouts of back pain, and when it happens, it is horrible! How do I manage it despite the excruciating pain? I try to keep moving, standing and walking as much as possible, I avoid doing things that flare it up, such as prolonged sitting, and I try not to let my catastrophic thoughts get the better of me. Mindfulness and relaxation strategies work wonderfully for that, thankfully. This is what I have learned from personal experience and learning the science. Let’s explore a bit more and find out what the science says?
Science says…
There is no magic cure for back pain! We already discussed that injections, opioids or surgery aren’t effective. What is left for the medical community to do? Oftentimes, less is more because the biggest predictor for future episodes of back pain, is previous back pain. Back pain is known to be recurrent and people usually get a flare up on average of once per year (Nicholls et al, 2011).
A systematic review by (Artus et al, 2010) which included 118 trials came to the conclusion that most back pain followed a standard pattern. Significant pain followed by a rapid improvement and then a plateau of symptoms irrespective of treatment. What this suggests is that long-term, most people improve along a relatively predictable timeline regardless of whether they get treatment or not. However, the severity of their suffering during this time period relies on some complex mechanisms. Patient preference for treatment and the communication between therapist and patient are extremely influential at determining treatment responses. The non-specific contextual effects and how these mechanisms influence patient outcomes is beyond the scope of this article. That article is currently in the works…
As healthcare providers, what are we supposed to do when presented with cases of low back pain? If the research suggests that it doesn’t matter what we do, people get better so does this mean we should we do nothing? How do we best manage these clients so they can more comfortably return to the activities they desire?
I think the first thing we need to do as healthcare professionals is change our thought processes. Changing how we think about back pain results in a different treatment and management approach. Applying an acute care model for any persistent musculoskeletal problem contradicts biology and is not evidence-based. Adoption of a chronic-care model that involves patient involvement and includes graded exercises programs, social supports, gradual return to work and accurate education about expectations for how to manage symptoms rather than fight against them is supported by evidence and has the benefit of being low risk of harm (Hayden et al, 2005, Hoffmann et al, 2007, & Staal et al, 2004).
Yellow flags – psychological risk factors
This topic is often controversial in the manual and movement therapy world. By acknowledging human psychology we are not being psychologists or counsellors. We are recognizing there could be factors other than biomechanical or tissue health impacting people’s pain related disability. There is a consistent relationship between psychological factors and the onset of pain and the transition from acute to persistent pain states (Nicholas et al, 2011). Acknowledging that stress, anxiety, depressed mood, fear-avoidance beliefs, catastrophic thoughts and passive coping strategies are associated with worse outcomes is following the evidence and empowers us with the understanding on how to better treat the person in front of us and not just their perceived mechanical dysfunctions and joint faults.
Addressing some of these obstacles to recovery is easily within scope of practice for any manual or movement therapist. For example, asking about pain beliefs, informing on the importance of active coping strategies, recognizing there are multiple factors in life which might be amplifying back pain all easily fit within our standard treatment interactions (Main & George, 2011).
Clinical practice guidelines
Following clinical practice guidelines (CPG’s) for low back pain is a simple way to decide what is the best course of action for your patient. A CPG is an amalgamation of the current best evidence. They are created to avoid the use of low quality or potentially harmful interventions and to highlight to therapists what the best strategies for success are. The first step is ruling out any major red flag for treatment. In that absence and the lack of radicular symptoms, treatment and management by a manual or movement therapist can begin.
According to a recent narrative review of low back pain guidelines by (O’Connell at al, 2017) the best strategies are to do something, because this is better than nothing. As long as the something you do isn’t harmful. Management should be provided with good quality evidence informed education which incorporates reassurance about their safety. If they are open to the discussion, introducing some pain science and the biopsychosocial domains about the complexity of back pain can be helpful for some. The other recommendation which is consistent across all MSK treatment guidelines is physical exercise, within tolerance. This doesn’t have to be strenuous. It could be as simple as walking, stretching, or doing simple activities that encourage movement in the affected area(s).
Despite the widespread suffering that spinal pain causes throughout the world, the management of it is fairly simple. From what I have learned over the years the following is a simple strategy to follow:
- Validate their pain experience
- Reassure that it is nothing serious
- Provide education that reduces fear and anxiety
- Encourage them to keep active and engage in as many physical activities that they can tolerate
- Use our manual skills as needed to help decrease pain sensitivity and encourage wellness.
Conclusion
The overcomplicating of normal painful experiences where the therapist searches for a cause will often lead to passive coping mechanisms, unhelpful beliefs about how the human body functions, and an over reliance on the therapist as the fixer of their pain rather than the therapist working as a facilitator to encourage self-management and well-being. Pain is complex, but it is common, let’s think simple and focus on the human in front of us and work with them, not on them to determine what they need to return to a happier and more functional life.